GE Healthcare
Adequacy of Anaesthesia (AoA) concept
The GE Healthcare Adequacy of Anaesthesia (AoA) concept helps clinicians deliver an individually tailored anesthesia and may help in their goal to improve patients’ outcomes.
 Adequacy of Anaesthesia (AoA) is a concept made up of various parameters to help clinicians assess patients’ individual responses to the delivery of inhaled and intravenous hypnotics, opioids, and NMBAs during general anaesthesia.
Adequacy of Anaesthesia (AoA) is a concept made up of various parameters to help clinicians assess patients’ individual responses to the delivery of inhaled and intravenous hypnotics, opioids, and NMBAs during general anaesthesia.
Learn more about AoA perioperative outcomes.
The AoA concept was designed to address the different components required for general anaesthesia. Indeed, AoA parameters provide continuous non-invasive measurement of:
- The state of the brain with SPECTRAL ENTROPY™
- Patient’s response to surgical stimuli and analgesic medications with SURGICAL PLETH INDEX (SPI)™
- Muscle relaxation/recovery with NEUROMUSCULAR TRANSMISSION (NMT)
Perioperative outcomes
The increase in elderly and obese patients undergoing major surgery represents a new challenge for anaesthesiologists who may struggle to determine the appropriate drug dosing for such complex patients.
The AoA concept was designed to enable clinicians to accurately personalize anaesthesia delivery, helping lower the risk of complications during and after surgery in all types of patients, including in the most vulnerable patients as mentioned above.
Hear from Prof. Berthold Bein, Head of Anaesthesiology & Intensive Care Dpt, Asklepios Klinik St. Georg, Hamburg (GER) explaining how the AoA concept can help optimise drug dosing in obese patients:
Entropy Monitoring
According to the NAP5 report, the incidence of Accidental Awareness during General Anaesthesia (AAGA) is ~1:8,000 when neuromuscular blockade was used and they are associated with psychological consequences for the patients experiencing them as 51% of episodes led to distress and 41% to longer-term psychological harm.
 In order to prevent such episodes, in particular when neuromuscular blockade isused or in patients who are judged to have high risk of AAGA for other reasons, the use of depth of anaesthesia monitoring, such as the Entropy monitoring, is recommended.
In order to prevent such episodes, in particular when neuromuscular blockade isused or in patients who are judged to have high risk of AAGA for other reasons, the use of depth of anaesthesia monitoring, such as the Entropy monitoring, is recommended.
The Entropy measurement may be used as an aid in monitoring the effects of certain anaesthetic agents. It is based on data acquisition and processing of raw electroencephalographic signals (State Entropy = SE) and frontal electromyographic signals (Response Entropy = RE).
The recommended range for both RE and SE is from 40-60, therefore a decrease of SE below 40 may indicate a too deep anaesthesia while an increase above 60 may indicate the need for adjusted titration.
In adults, studies have shown that entropy monitoring may help the user titrate anaesthetic drugs according to the individual needs and may be associated with a reduction of anaesthetic use and faster emergence from anaesthesia.
SPI Monitoring
Several studies reported fewer unwanted events, reduced opioid consumption and shorter emergence from anaesthesia, when opioid administration was based upon monitoring of the nociceptive-anti-nociceptive balance.
 The Surgical Pleth Index (SPI)* is a parameter that reacts to haemodynamic responses caused by surgical stimuli and analgesic medications. SPI is an algorithm that uses two components of the GE photoplethysmographic signal when measured on GE SpO2 finger sensors only.
The Surgical Pleth Index (SPI)* is a parameter that reacts to haemodynamic responses caused by surgical stimuli and analgesic medications. SPI is an algorithm that uses two components of the GE photoplethysmographic signal when measured on GE SpO2 finger sensors only.
By observing the SPI value and trend, clinicians can monitor real time adult patient’s responses to surgical stimuli and analgesic medications therefore saving valuable time for optimization analgesia delivery.
The optimal SPI target has not been recommended yet as more studies need to prove the clinically relevant range of SPI measurements. However, in several studies, a range of [20; 50] has been considered for guiding opioids titration.
Published literature suggests that SPI-guided anaesthesia may result in lower remifentanil consumption, more stable haemodynamics and lower incidence of unwanted events.
NMT Monitoring
Post-Operative Residual Curarization (PORC) incidence in post-anaesthesia care units (PACU) is estimated to be up to 45% after a single shot muscle relaxation1. Considering that about 230 millions of patients undergo a major surgery each year, about 100 patients per minute would suffer from discomfort, reduced ventilation capacity, double vision and a 4-to-5 times increased aspiration risk (see Fig X). Such residual effects have clinical consequences and complications that can prolong hospitalization, particularly in vulnerable population such as obese patients.

Fig. XAccording to Prof. Jan Paul Mulier, AZ Sint Jan Hospital, Belgium, NMT monitoring is key to prevent respiratory complications in obese patients: listen to Prof. Jan Paul Mulier explaining why Neuromuscular Transmission monitoring is essential to optimize muscle relaxation in this challenging population.
GE NMT monitoring technology
 Electromyography (EMG) is the process of recording the specific electrical muscular fibers activity in response to ulnar nerve stimulation.
Electromyography (EMG) is the process of recording the specific electrical muscular fibers activity in response to ulnar nerve stimulation.
Kinemyography (KMG) uses a mechanoSensor and quantifies the evoked mechanical response by measuring the motion of the thumb by a piezoelectric sensor, which converts the physical motion to an electrical signal.
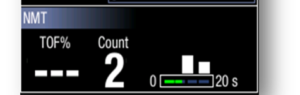 Adequate recovery from neuromuscular block, indicated by TOF>90%, can be reliably determined only with a quantitative measurement. EMG TOF ratio is an alternative gold standard, after Mechanomyography (MMG), for detecting neuromuscular block in clinical setting and is not interchangeable with Acceleromyography (ACG) TOF.
Adequate recovery from neuromuscular block, indicated by TOF>90%, can be reliably determined only with a quantitative measurement. EMG TOF ratio is an alternative gold standard, after Mechanomyography (MMG), for detecting neuromuscular block in clinical setting and is not interchangeable with Acceleromyography (ACG) TOF.
Published literature suggests that quantitative measurement of neuromuscular transmission is the only recommended method to diagnose residual block1. Indeed, NMT measurements may help the clinician optimize dosage during anaesthesia1 and optimize recovery and prevention of respiratory complications in PACU.
Decision support tool
 The configurable AoA split screen of GE’s CARESCAPE modular monitors, combined with haemodynamic parameters and respiratory gas measurements, provides a comprehensive visual view of patient’s status.
The configurable AoA split screen of GE’s CARESCAPE modular monitors, combined with haemodynamic parameters and respiratory gas measurements, provides a comprehensive visual view of patient’s status.
In the unique AoA split screen, you will find the BalanceView, which combines and plots Surgical Pleth Index (SPI) and SE values (one component of the Entropy measurement).
When seconds counts in an intensive and multitasking environment, the BalanceView is guidance for prompt visualization of the patients’ responses to changes of anaesthesia conditions and may help save valuable time on responsiveness to analgesia/depth of anaesthesia optimization for each individual patient.
The “white dot” that moves drastically away from the target zone may indicate inadequate hypnosis or analgesia level.